GASTRITIS: THE MOST COMMON CAUSE
Gastritis is an inflammation of the lining (mucosa) of the stomach. Gastritis can be caused by irritation due to excessive alcohol use, chronic vomiting, stress, or use of certain medications such as aspirin or other inflammatory drugs. It may also be caused by:
- Infections: bacteria and virus
- Bile reflux
The most common cause of gastritis is due to a bacterium called Helicobacter pylori (HP). HP is a spiral-shaped, gram-negative bacterium that has adapted to thrive in acid. It was identified by two Australian doctors, Barry Marshall and Robin Warren, in 1982. They got the Nobel Prize for their discovery in 2005.
HP have coexisted with humans for many thousands of years, and infection with this bacterium is common. The Centers for Disease Control and Prevention estimates that approximately two-thirds of the world’s population harbors the bacterium.
The stomach produces an acid called hydrochloric acid (HCl) and this normally kill most of the living organism entering the stomach, but not HP which can live and proliferate in the acid environment because they produce ammonium that surrounds the bacteria as a “cloud” and protect them against the acid (HCl). In addition, the helical shape of HP allows it to burrow into the mucus layer, which is less acidic than the inside space, or lumen, of the stomach.
In developing countries, HP commonly causes chronic infections and is usually acquired during childhood. In western countries, infection is less common among children but increases with age.
Most people don’t realize they have HP infection because they never get sick from it. If you develop signs and symptoms of a peptic ulcer, your doctor will probably test you for HP infection. If you have HP infection, it can be treated with antibiotics.
A number of other symptoms may be associated with H. pylori infection, including:
- excessive burping or belching
- feeling bloated
- nausea
- heartburn
- fever
- lack of appetite, or anorexia
- unexplained weight loss
HOW DO WE GET INFECTED?
The exact way HP infects someone is still unknown. HP bacteria may be passed from person to person through direct contact with saliva, vomit or fecal matter. HP may also be spread through contaminated food or water.
DIAGNOSIS
The doctor will often suspect that you have gastritis after talking with you and has several ways to confirm if you have gastritis caused by HB or not.
Diagnostic tests are usually divided into noninvasive methods and invasive (endoscopic-based).
Non-invasive diagnostic tests include:
Urea breath test, stool antigen test, serological, and molecular examinations.
- Blood test. Analysis of a blood sample may reveal evidence of an active or previous HP infection in your body. Because the serological tests do not distinguish between active infection and past exposure to HP, further confirmation by other tests is required before eradication therapy.
- Breath test. A breath test for HP infection – this involves drinking a glass of clear, tasteless liquid that contains radioactive carbon and blowing into a bag. If you have an HP infection, carbon is released when the solution is broken down in your stomach. Your body absorbs the carbon and expels it when you exhale. You exhale into a bag, and your doctor uses a special device to detect the carbon molecules.
- Stool antigen test. A laboratory test called a stool antigen test looks for foreign proteins (antigens) associated with HP infection in your stool.
Invasive diagnostic tests include:
Endoscopic image, histology, rapid urease test, culture, and molecular methods.
- Endoscopy. Is usually performed to diagnose HP-associated diseases, such as peptic ulcer diseases, atrophic gastritis, MALT lymphoma and gastric cancer.
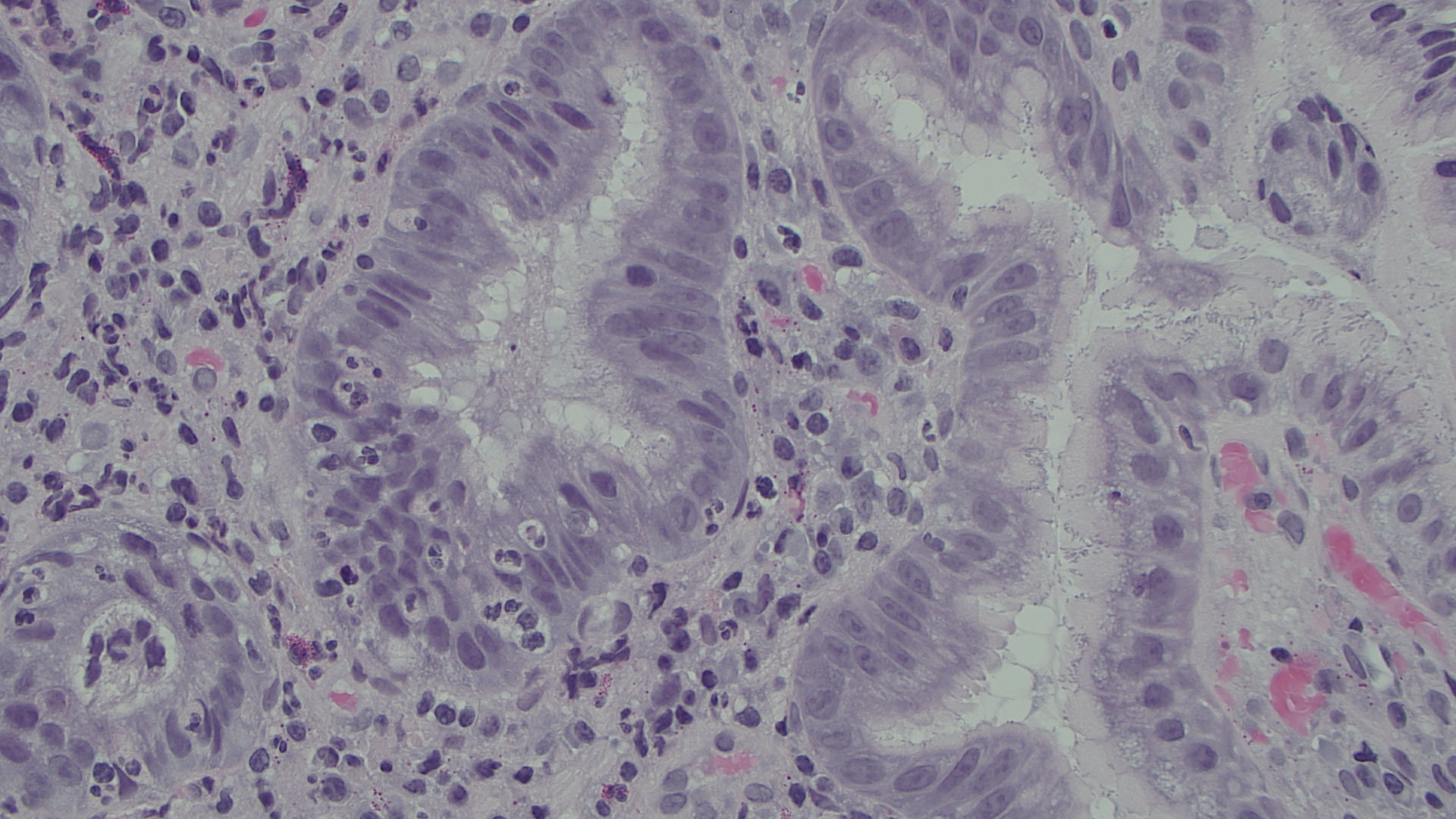
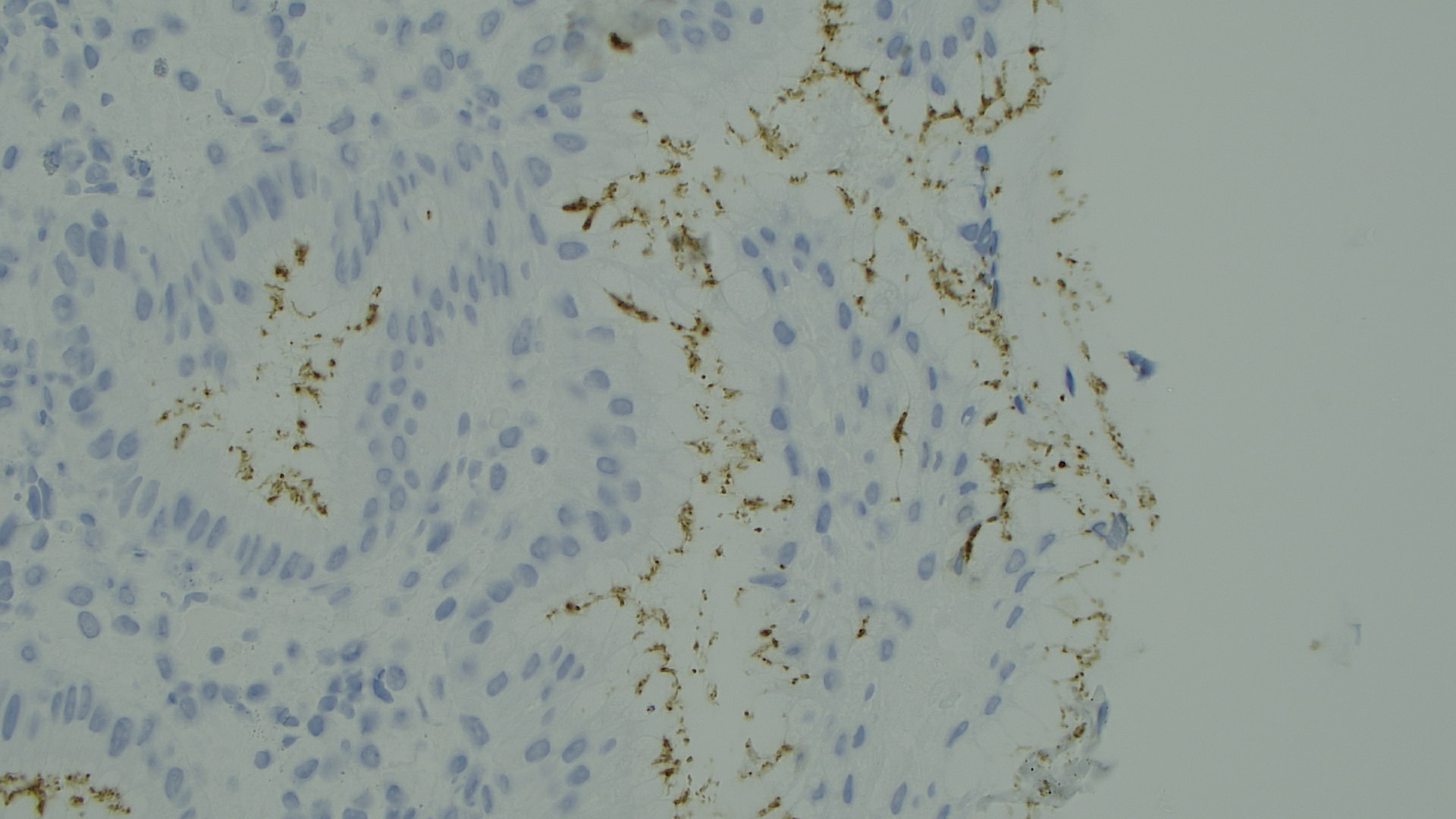
- Histology. Histology is usually considered to be the gold standard in the direct detection of HP infection and is also the first method used for the detection of HP. However, several factors influence the diagnostic accuracy of histology, such as site, size and number of biopsies, and staining methods. Staining is the critical part of the histological examination. Many laboratories use HE staining and immunohistochemical stain.
This is an HE stain of the gastric mucosa where it is possible to see Helicobacter pylori bacterias.
This is an immunohistochemical stain against Helicobacter Pylori where you easily can see the bacterias as brownly small twisted rods. The immunohistochemical stain is the most sensitive and specific stain.
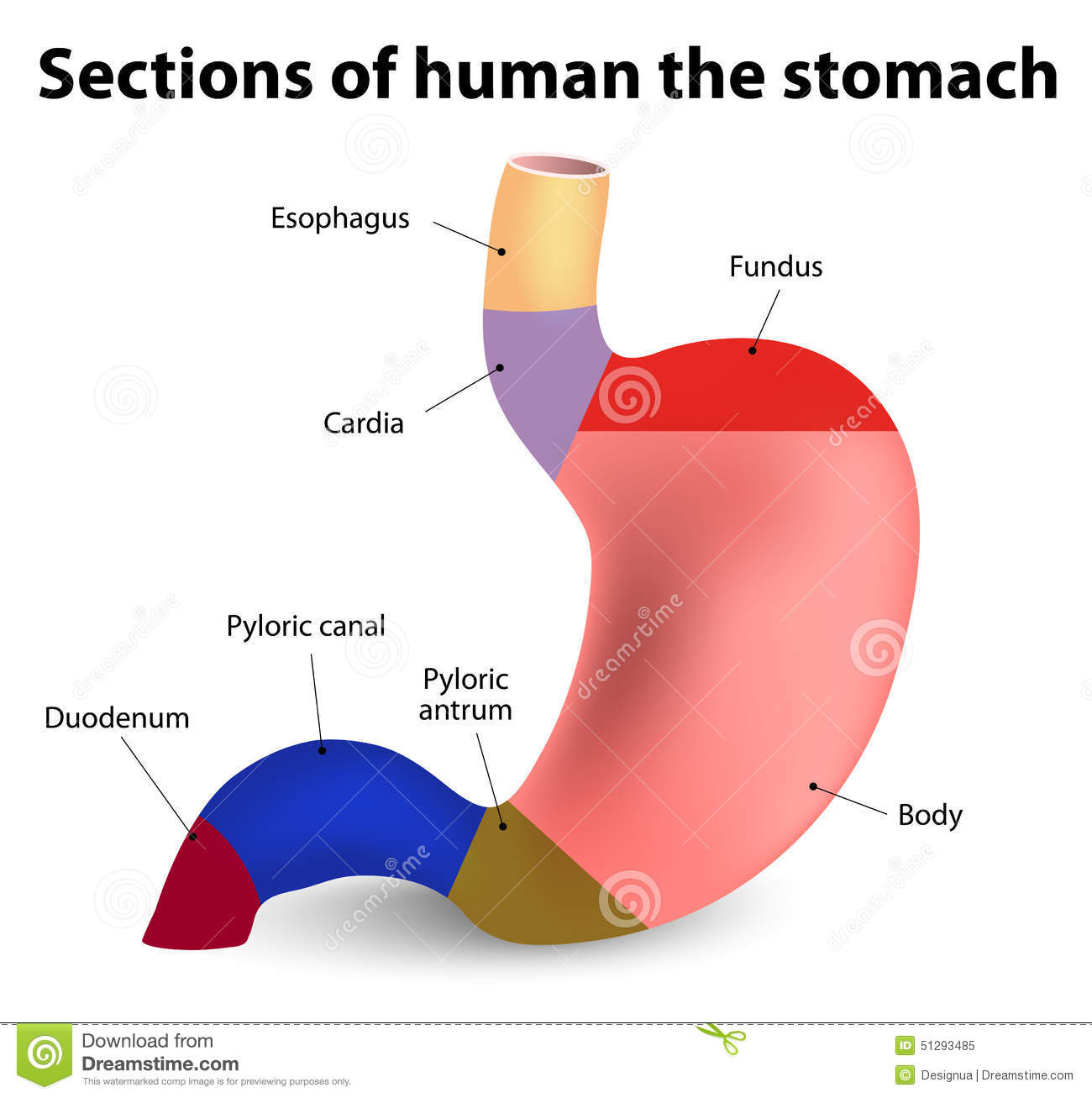
- Rapid urease test. For routine clinical practice, rapid urease test (RUT) is the most useful invasive test for the diagnosis of HP infection because it is inexpensive, rapid, easy to perform, highly specific and widely available. The test is performed at the time of gastroscopy. A biopsy of mucosa is taken from the antrum of the stomach, and is placed into a medium containing urea and an indicator such as phenol red. The urease produced by H. pylori hydrolyzes urea to ammonia, which raises the pH of the medium, and changes the color of the specimen from yellow (negative) to red (positive).
- Culture. Culturing of HP from gastric biopsy specimen is a highly specific but less sensitive method. Although culture is a time-consuming, expensive and laborious test for diagnosis, the antibiotic sensitivity test of HP provided by culture is a particular advantage in clinical practice.
- Polymerase chain reaction. Since the application of polymerase chain reaction (PCR) to detect H. pylori infection, PCR has been used extensively for the diagnosis of H. pylori from gastric biopsy specimens, saliva, stool, gastric juice and variable specimens. PCR provides excellent sensitivity and specificity, greater than 95%, as compared with other conventional tests and has more accurate results of detecting H. pylori in patients with bleeding.
COMPLICATIONS
Complications associated with HP infection include:
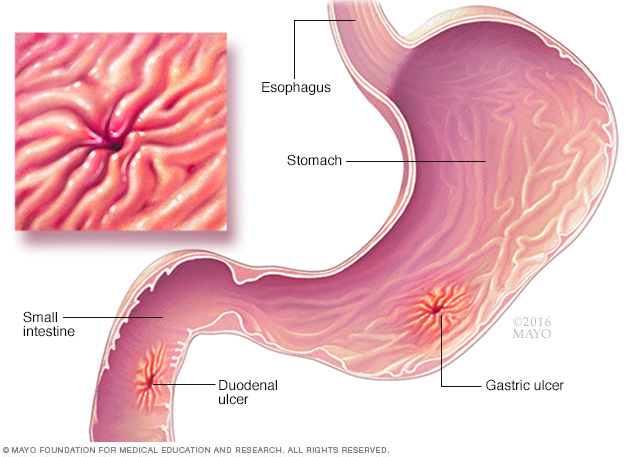
1. Ulcers.
HP can damage the protective lining of your stomach and small intestine. This can allow stomach acid to create an open sore (ulcer). About 10 % of people with HP will develop an ulcer.
2. Inflammation of the stomach lining.
H. pylori infection can irritate your stomach, causing inflammation (gastritis).
3. Stomach cancer.
The International Agency for Research on Cancer classifies HP as a carcinogen, or cancer-causing agent, in humans. It has been accepted that colonization of the stomach with HP is an important cause of gastric cancer and of gastric mucosa-associated lymphoid tissue (MALT) lymphoma.
Prevention
In areas of the world where HP infection and its complications are common, doctors sometimes test healthy people for HP. Whether there is a benefit to treating HP when you have no signs or symptoms of infection is controversial among doctors.
People who have active gastric or duodenal ulcers or a documented history of ulcers should be tested for HP, and, if they are infected, should be treated.
References:
- WebMD
- Mayo Clinic
- Nacional Cancer Institute
- World J Gastroenterol. 2015 Oct 28; 21(40): 11221–11235.
About the Author Kjell H Kjellevold
A doctor and specialist in pathology. He has always been concerned about health and how to manage a good and healthy lifestyle. The blog will mainly be about the use of essential oils, health, and training.